
Dry eye, also referred to as dry eye disease (DED) or dry eye syndrome, arises when the eyes fail to produce sufficient tears or when the quality of those tears is inadequate. This might sound trivial, but tears are the unsung heroes of eye health. They keep the eyes lubricated, comfortable, and protected. Without them, the eyes face not only discomfort but also potential damage and susceptibility to infections.
How Tears Work: The Essential Trio
Tears aren’t just water rolling down your cheeks when you’re emotional. They’re complex and fascinating, composed of three distinct layers:
- Oily Layer
This is the outermost layer of the tear film, originating from the meibomian glands in the eyelids. Its main job? To keep tears from evaporating too quickly. Think of it as the “seal” that locks moisture in while ensuring the tear surface remains smooth. - Watery Layer
Sandwiched between the oily and mucus layers, this layer makes up the bulk of your tears. Produced by the lacrimal glands, it cleans the eye by flushing out debris and unwelcome particles. It’s like your eye’s built-in rinse cycle. - Mucus Layer
The innermost layer, crafted by goblet cells in the conjunctiva, ensures that the watery layer spreads evenly across the surface of your eye. Without this adhesive-like component, tears wouldn’t stay put, leaving your eyes parched and exposed.
Each of these layers has its own role, but they work together seamlessly—until something disrupts the balance.
Tear Production and Distribution: The Blink Connection
Tear production isn’t a passive process. It’s a well-coordinated effort involving the lacrimal glands and your body’s natural blinking reflex. Each blink acts like a tiny squeegee, spreading tears evenly across the eye’s surface. It’s an intricate system designed to keep the eye hydrated and protected from the environment.
Tear Preservation: The Role of Meibomian Glands and Punctum
Preservation of tears is equally important. The meibomian glands, responsible for the oily layer, prevent tears from evaporating prematurely. Meanwhile, the punctum—small drainage channels located in the corners of your eyelids—regulates tear outflow. If the balance tilts too far in favor of drainage or evaporation, dryness ensues.
Ocular Surface Disease: When Balance Is Lost
Ocular Surface Disease (OSD) goes hand in hand with dry eye. While dry eye might seem like a standalone issue, it’s often a symptom of a more complex underlying problem: damage to the corneal surface. The cornea, which relies on the tear film for nourishment and protection, can suffer significantly when tears are deficient in quality or quantity. This damage not only causes discomfort but, if left untreated, can lead to more severe complications, including permanent vision loss.
While dry eye is a common form of OSD, it isn’t the only one. Allergies, autoimmune conditions like Sjögren’s syndrome, eyelid inflammation (blepharitis), and environmental factors all play a role in disrupting tear film balance and contributing to ocular surface disease.
Dry Eye Symptoms: How They Feel, Look, and Affect You
Dry eye symptoms aren’t always straightforward. You might feel one thing and see another, and some signs might seem downright contradictory—like watery eyes being a symptom of dryness. Let’s break it down into clear categories to help you understand what’s happening.
Most Common Dry Eye Symptoms
- Dryness
The hallmark symptom, dryness, feels like your eyes are screaming for moisture. It can range from mild irritation to an intense, unrelenting sensation of parched discomfort. - Burning or Pain
A sharp, stinging sensation or a constant dull ache can be common. Think of it like the way your skin feels after being exposed to harsh wind—raw and tender. - Redness
Red, bloodshot eyes signal inflammation and irritation, often making you look as tired as your eyes feel. - Itching
Itchy eyes can make you want to rub them, but beware: this can worsen irritation and lead to further complications. - Foreign Body Sensation
Ever feel like there’s something stuck in your eye, even when there isn’t? This gritty or sandy feeling is a classic sign of dry eye. - Watery Eyes
It may seem counterintuitive, but watery eyes—known as reflex tearing—are your body’s desperate attempt to compensate for dryness. Unfortunately, these tears lack the proper balance to hydrate your eyes effectively. - Discomfort
A vague but persistent sense of something being “off” in your eyes. It’s not always easy to describe, but you know it when you feel it.
Vision-Related Symptoms
Dry eye doesn’t just cause discomfort—it messes with how you see the world.
- Blurry or Fluctuating Vision
Dry eye disrupts the tear film, which is vital for clear vision. This can cause your sight to go in and out of focus, especially when reading, using screens, or driving at night. - Light Sensitivity (Photophobia)
Bright lights can feel unbearable, making it hard to be outdoors on sunny days or under fluorescent lights indoors. - Glare or Halos Around Lights
Seeing halos or glare, especially at night, is another sign of tear film instability. This can make driving after dark particularly challenging.
Physical Signs of Dry Eye
- Watery Eyes (Reflex Tearing)
Excessive tearing might fool you into thinking your eyes are well-lubricated, but it’s a sign of irritation rather than hydration. - Redness
Inflammation in the eye makes redness a common physical marker of dry eye syndrome. - Sticky or Stringy Discharge
You might notice mucus-like strands in or around your eyes, a result of tear film imbalance. - Crusting Around Eyelids in the Morning
Waking up with crusty eyelids or lashes is another indicator. This crust often forms as the tear film tries to compensate overnight.
The Overlap of Symptoms: Why They Vary So Much
You might notice that some symptoms seem contradictory or overlap. For example, how can your eyes feel dry but still water excessively? This happens because dry eye disrupts the delicate tear film, triggering your body to overproduce tears that are lacking the necessary balance of water, oil, and mucus. Unfortunately, these reflex tears evaporate too quickly or fail to spread evenly, leaving your eyes in worse shape.
By understanding these symptoms and their causes, you can work with our eye doctors to find solutions that restore balance and comfort to your eyes.
What Causes Dry Eye? Disruptions in Tear Balance
Dry eye results from factors that interfere with the production, quality, or retention of tears. Here’s a closer look at common causes:
Age-Related Changes
Tear production naturally declines with age. Combined with changes in eyelid and gland function, this makes older adults more prone to dry eye.
Hormonal Fluctuations
Hormones significantly influence tear production. Events like pregnancy, menopause, or using oral contraceptives can disrupt tear quality and quantity, especially for women.
Medication Side Effects
Several medications can reduce tear production, including:
Structural and Mechanical Issues
Health Conditions
Systemic conditions affecting tear production include:
Environmental and Lifestyle Factors
- Environmental Exposures: Dry, windy, or smoky environments increase tear evaporation.
- Screen Time: Reduced blinking during screen use disrupts tear distribution.
- Contact Lenses: Long-term use interferes with the natural tear film.
- Refractive Surgery: Procedures like LASIK may affect tear production reflexes.
From internal changes like aging and medication use to external factors like harsh environments or prolonged screen time, the causes of dry eye are diverse but interconnected. Recognizing these triggers can help manage symptoms effectively and guide treatment tailored to individual needs.

Dry Eye Diagnosis: A Thorough Evaluation
When dry eye symptoms begin to interfere with your daily life, the first step to relief is a comprehensive evaluation. Dry eye isn’t one-size-fits-all; it has multiple potential causes. Understanding the root of your symptoms requires looking at the problem from all angles—tear quantity, quality, evaporation, and contributing factors like inflammation or eyelid conditions.
Getting to the Root Cause of Symptoms
- Tear Quantity
Measuring the amount of tears produced is a crucial starting point. Tests like the Schirmer’s test use small strips of paper to assess tear production. If the volume is too low, it could point to a problem with the lacrimal glands. - Tear Quality
Tears aren’t just water; they’re a complex mix of water, oil, and mucus. Poor quality tears—lacking in any one of these layers—may fail to coat the eye properly, leading to symptoms like blurriness and irritation. - Evaporation
A tear’s lifespan on your eye matters. Testing the tear break-up time (TBUT) evaluates how quickly tears evaporate. Rapid evaporation often signals problems with the meibomian glands, responsible for producing the oily layer of the tear film. - Contributing Factors
Conditions like blepharitis (eyelid inflammation) or systemic inflammation can exacerbate dry eye. Additionally, eyelid structure and blinking patterns are examined for their role in distributing tears effectively. - Patient History and Gland Health
Our eye doctor will ask about your symptoms, lifestyle, and medical history to uncover patterns. Do you spend long hours on screens? Do you take medications known to dry the eyes? These clues, paired with an in-office evaluation of your lacrimal and meibomian glands, help pinpoint the source of your discomfort.
What is InflammaDry and Why It Matters for Dry Eye
If you’re struggling with dry, irritated eyes and wondering why over-the-counter drops just aren’t cutting it, you’re not alone. Dry eye isn’t always just about tear volume, it’s often driven by inflammation beneath the surface. That’s where InflammaDry comes in. It’s a quick, in-office test that checks for a specific inflammatory marker called MMP-9, which tends to spike when the surface of your eye is inflamed. The test is painless and gives results in about 10 minutes. Why is this helpful? Because if inflammation is playing a big role in your symptoms, our eye doctors can tailor the treatment recommendations, including treatments such as IPL that target inflammation. Think of it as a smarter way to match the treatment to what’s really going on. Not every case of dry eye looks the same, and InflammaDry helps us see the difference.

Looking for an Experienced Dry Eye Doctor in Orange County?
At Insight Vision Center Optometry, we combine state-of-the-art technology with personalized care to provide the most advanced dry eye treatments in Orange County. Our team of advanced optometrists is skilled in diagnosing and addressing even the most complex cases of dry eye. We take the time to understand your unique symptoms and lifestyle, ensuring a tailored treatment plan designed to restore your eye health and quality of life. Whether you need innovative therapies like IPL or the unparalleled comfort of scleral lenses, we are committed to helping you see and feel your best. Choose us for compassionate care, cutting-edge solutions, and a commitment to excellence in eye health.
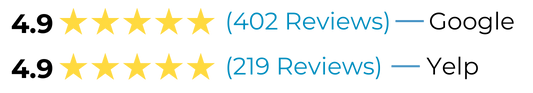
The Highest Rated Advanced Eye Care Center In Orange County
What Our Patients are Saying
“I love this office! The staff is so friendly, helpful, and welcoming. Dr. Lam has helped with my dry eye symptoms and myopia and takes the time to explain things thoroughly. I never feel like she is rushing me out of the office to see the next patient. She is extremely knowledgeable and I feel very well cared for. I highly recommend this office!”
⭐⭐⭐⭐⭐
“More recently I had an issue with super dry eyes and they provided me multiple solutions and care instructions to heal them quickly. What I like is that it’s not all about just solving the issue, they taught me about long term care and what to change to ensure my eyes get the hydration they need.”
⭐⭐⭐⭐⭐
Dry Eye Treatment: Finding the Right Solution
Treating dry eye isn’t just about masking the symptoms—it’s about addressing the root cause. A personalized approach, tailored to your specific diagnosis, often combines lifestyle changes, targeted therapies, and ongoing care.
Lifestyle Changes: Small Steps, Big Impact
- Omega-3 Fatty Acids
Adding omega-3s to your diet, through foods like fish or supplements, can help improve the quality of the oily layer in your tears. This strengthens the tear film and reduces evaporation. - Warm Compresses
Regularly applying warm compresses can unclog the meibomian glands, boosting tear quality. - Reducing Screen Time and Blinking Exercises
If prolonged screen use is a factor, taking breaks and limiting screen time can encourage blinking and relieve eye strain. Conscious blinking during screen use can also improve tear distribution. - Environmental Changes
Use a humidifier to counteract dry air from heating or air conditioning. Minimizing exposure to wind, smoke, and other irritants also makes a big difference. - Hydration
Staying well-hydrated by drinking enough water daily helps your body produce healthy tears.
Keeping Tears and Moisture Where They Belong
- Eye Drops
Artificial tears are a quick, temporary fix. While they provide immediate relief, they may not address the underlying cause of dryness. - Punctal Plugs
These tiny devices are inserted into the tear drainage ducts (puncta) to slow tear loss, keeping moisture on your eyes longer. - Reducing Evaporation
Treatments for meibomian gland dysfunction (MGD) include warm compresses, in-office procedures like LipiFlow, and specially formulated eye drops. - Moisture Goggles
For severe dry eye, moisture goggles create a humid environment around your eyes, reducing evaporation and providing lasting comfort. - Scleral Lenses
These advanced contact lenses vault over the cornea, trapping a reservoir of fluid that keeps the eye surface hydrated all day.
Increasing Tear Production
Prescription medications like Restasis (cyclosporine) or Xiidra (lifitegrast) can stimulate your lacrimal glands to produce more tears. These medications also help combat underlying inflammation, improving overall tear stability.
Stabilizing the Ocular Surface and Treating Contributing Conditions
- Eyelid Health
Addressing issues like blepharitis with lid scrubs or medicated wipes can improve tear film stability. - Topical Steroids
Short courses of topical steroids help reduce inflammation, providing relief for symptoms that stem from chronic irritation. - Amniotic Membranes
For severe cases, amniotic membrane treatments help heal the ocular surface by delivering anti-inflammatory and regenerative properties. - Autologous Serum Eye Drops
Made from your own blood, these customized drops are rich in growth factors and nutrients, offering a powerful treatment for chronic or refractory dry eye.
Heating and Expression of the Glands: Restoring Balance to the Tear Film
One of the most common culprits behind dry eye is meibomian gland dysfunction (MGD), a condition where the tiny oil-producing glands in the eyelids (meibomian glands) fail to function properly. These glands are critical for producing the oily layer of your tear film, which slows evaporation and maintains stability. When MGD is left untreated, the glands can become clogged, leading to inflammation, reduced tear quality, and, over time, gland atrophy—a permanent loss that further compromises eye health.
Why Treating MGD Matters: Preserving the Glands
The importance of treating MGD cannot be overstated. These glands are not regenerative, meaning that once they atrophy, they are gone for good. Without the lipid layer they produce, tears evaporate too quickly, creating a cycle of dryness, irritation, and inflammation. This ongoing damage can result in:
- Progressive dry eye symptoms: Increased discomfort, blurry vision, and light sensitivity.
- Ocular surface damage: Chronic exposure due to tear instability can harm the cornea, leading to complications like scarring and vision loss.
- Diminished quality of life: Unmanaged MGD can significantly impair daily activities like reading, driving, or using screens.
Early intervention is crucial to preserve gland function and maintain a stable, healthy tear film.
TearCare: In-Office Treatment for MGD
TearCare is an advanced, non-invasive treatment specifically designed to address MGD by targeting the underlying blockage of the meibomian glands. Here’s how it works:
Precise Heating
The TearCare system uses smart, flexible devices placed on the eyelids to deliver controlled heat directly to the meibomian glands. This gentle warmth softens and loosens hardened oil (meibum) that clogs the glands, preparing them for expression.
Effective Expression
After the heating phase, your eye care provider manually expresses the glands, ensuring the removal of accumulated blockages. This restores normal gland function, allowing them to produce the essential oils needed for a healthy tear film.
Customization
TearCare is tailored to each patient, addressing the specific degree of gland dysfunction. Its flexibility and comfort make it suitable for most individuals, even those with severe MGD.
Benefits of TearCare:
Intense Pulsed Light (IPL): A Comprehensive Solution
Intense Pulsed Light (IPL) therapy is another effective in-office treatment for MGD and associated inflammation. Originally developed for skin conditions like rosacea, IPL has been adapted for ocular use due to its remarkable ability to address multiple factors contributing to dry eye.
- Targeting Inflammation
IPL uses specific wavelengths of light to reduce inflammation, a key driver of MGD and ocular surface disease. By targeting inflammatory blood vessels around the eyelids, IPL helps to calm redness and irritation. - Improving Meibomian Gland Function
The heat generated by IPL liquefies clogged meibum, facilitating its release. This enhances the glands’ ability to produce and secrete the vital lipid layer of the tear film. - Antimicrobial Effects
IPL also kills Demodex mites, a common contributor to blepharitis and MGD. These mites exacerbate gland dysfunction by blocking gland openings and triggering inflammation.
Benefits of IPL:
Choosing the Right Treatment for MGD
Both TearCare and IPL are highly effective in addressing MGD, but their choice depends on the severity of gland dysfunction and individual patient needs. Regular follow-ups and maintenance treatments can ensure long-lasting relief and prevent irreversible damage. By targeting the root cause of dry eye—meibomian gland dysfunction—these treatments not only alleviate symptoms but also protect the long-term health of your eyes.
Scleral Lenses for Dry Eye Treatment: A Revolutionary Approach
Scleral lenses represent a transformative solution for individuals with chronic dry eye disease, particularly for those whose symptoms are severe and unresponsive to conventional treatments. Unlike standard contact lenses, scleral lenses are specially designed to address the unique challenges of dry eye by providing continuous hydration, protection, and stabilization of the ocular surface.
Scleral lenses are large-diameter, gas-permeable contact lenses that vault over the cornea and rest on the sclera (the white part of the eye). This design creates a unique reservoir of fluid between the lens and the cornea, offering several distinct advantages:
How Scleral Lenses Work for Dry Eye Treatment
The unique properties of scleral lenses make them a highly effective treatment for dry eye, particularly in severe or complex cases. Here’s how they address key aspects of the condition:
Stabilizing the Ocular Surface
For patients with corneal irregularities, such as those caused by keratoconjunctivitis or advanced dry eye, scleral lenses provide a stable surface that improves both comfort and vision.
Restoring the Tear Film
The tear reservoir beneath the lens compensates for the deficiencies in natural tear production, ensuring that the cornea remains moist and protected throughout the day.
Reducing Inflammation
By creating a physical barrier, scleral lenses help to minimize exposure to environmental triggers that cause inflammation, such as allergens or dry air.
Preventing Corneal Damage
Chronic dry eye can lead to corneal abrasions, ulcers, and even scarring. Scleral lenses protect the cornea from further damage, allowing the ocular surface to heal.

Experience Relief from Dry Eye Today! Visit Orange County’s Top Rated Advanced Eye Care Center
Don’t let dry eye disrupt your life any longer. Our advanced treatments, including TearCare, IPL, and scleral lenses, offer lasting relief tailored to your unique needs. Schedule your comprehensive dry eye evaluation today and take the first step toward clearer, more comfortable vision. Call us at (714) 942-1361 or book a dry eye evaluation with us online.
Call us at (714) 942-1361 to book your child’s appointment, or schedule online.





